Healthy Ethics for Health Policy: ISPS’s Interdisciplinary Center for Bioethics
When Americans began to exhale COVID-19 across the country in 2020, state governments scrambled to determine what it meant to shut down public gatherings and many services. Hospitals confronted the brunt of the immediate crisis, forced to ration supplies and equipment, implement safety measures, and define hierarchies of need for worst-case scenarios.
But there were dozens of other rules and regulations governing health care systems less dire than how to triage patients flooding intensive care units. The disease created massive staffing shortages across the economy, demanding decisions about, for example, whether the state can suspend a rule requiring how many hot meals nursing homes must serve each day.
In Connecticut, many of those decisions had been considered more than a decade earlier. Yale’s Interdisciplinary Center for Bioethics, supported by ISPS, participated in pandemic planning in the wake of the H1N1 bird flu and SARS outbreaks. When COVID-19 arrived, an adaptable framework for those policies was already in place.
These are the types of questions the center was designed to answer. Led by Stephen Latham, the Interdisciplinary Center for Bioethics explores ethical tensions across the globe and within law, policy, public health, the clinical setting, and other societal contexts. Programming engages not only with medical ethics but also with ethics relating to the environment, animals, research practices, business, and new technologies.
“Our number one mission is to teach,” Latham said. “We encourage informed discussion of the issues raised by our increasing powers over life, including issues of justice and rights, familial responsibility, corporate and state power, and what it means to live healthy and productive lives.”
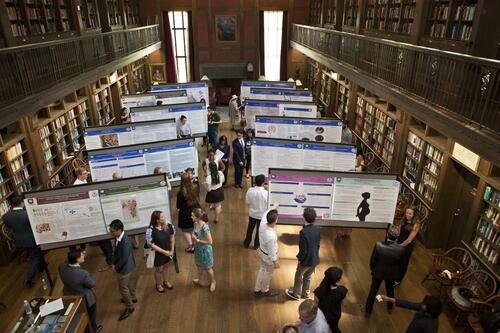
The center conducts the annual Sherwin B. Nuland Summer Institute in Bioethics, run by Associate Director Lori Bruce. This two-month program trains attendees in the fundamentals of bioethics and includes an introduction to ethical theory, ethical policymaking, bioethical principles, terms, and history, along with sessions on some of the most pressing bioethics topics today. Students attend live lectures, small-group seminars, career talks, and special events at Yale museums and The Hastings Center, a non-partisan independent bioethics research institute allied with the Yale Interdisciplinary Center for Bioethics. They also learn to work together in multidisciplinary teams and draw on each other’s strengths and differences.
With remote access increasing accessibility to the program over recent years, it has drawn about 150 students annually — including those who attend both the full program or a shorter foundational course — from over 30 countries and American colleges.
“In addition to our fantastic students, a really nice feature of the summer program is that we invite international faculty members — who in some cases may be one of very few who teach bioethics at their schools,” Latham said. “And they suddenly find themselves in a room with dozens of bioethicists, often ending up collaborating on papers and grant proposals. They get to hang out with people who do what they do.”
In addition, Lori Bruce co-chairs, and Latham is a member of, the Adult Ethics Committee at Yale New Haven Hospital. They are involved not only in providing ethical counsel to all committee members and guiding bedside ethics consultations, but also in the revision of hospital policies, such as those governing the appropriateness of patient treatment and when and how patients are discharged. Latham, as an institutional review board (IRB) chair, and Bruce, as an IRB member, regularly review human-subjects research protocols for Yale’s Human Research Protection Program, including protocols utilizing artificial intelligence.
As well as the earlier pandemic planning, the center served a key role in developing, monitoring, and adapting the New Haven Health System’s pandemic response policies after the COVID-19 outbreak in March 2020, which have helped navigate issues over resource allocation during periods of high hospitalization. Other recent activities have included participation in an advisory group to address uniform code status for the system’s hospitals and the decision to exclude a highly expensive Alzheimer’s disease drug with uncertain benefits from the system’s formulary.
“The percentage of hospitals that have ethics committees and deal with disputes that arise with care in hospitals is now as high as it’s ever been,” Latham said. “I think bioethics has established itself as a well-known field that institutions take seriously.”
The Interdisciplinary Center for Bioethics began as a program, comprised of Yale faculty members with common interests but no dedicated infrastructure or academic appointments. Its early governing board included Arthur Galston, a plant physiologist whose discovering of a potent herbicide was developed into Agent Orange and used during the Vietnam War to deprive enemy soldiers of food and vegetative cover. Galston spoke out against the military use of his discovery and its toxic environmental and health effects on the people of Vietnam and American war veterans.
The program became a center in 2005, and Latham joined the following year, embracing the broad focus beyond biomedical research and practice to include legal and environmental issues pioneered by Galston.
“Yale’s Interdisciplinary Center for Bioethics is unique because it isn’t housed at the medical school,” Latham said, noting that he collaborates often with Dr. Mark Mercurio, director of Yale School of Medicine’s Program for Bioethics, which focuses more on the ethics of biomedical research than clinical practice and law. “Undergraduate liberal arts majors so open-minded and very fun to teach.”
The center also serves as a resource for lawmakers.
In the culmination of a long legislative battle, Lori Bruce was invited by Connecticut elected officials to shine a light on the ethics of consent for intimate medical examinations. She gave public lectures explaining the ethical tensions, served on the state’s strategic task force, and conducted a national survey — the first of its kind — that helped instigate the passage of Connecticut’s 2022 bill requiring explicit consent for these examinations.
“The Interdisciplinary Center for Bioethics is a great example of ISPS’s commitment to research that produces practical results to improve our world,” said Alan Gerber, ISPS director and Sterling Professor of Political Science. “These are some of the hardest questions we face as a society, and it is crucial to have experts engaging in thoughtful analysis so we can craft safe, effective, and ethical policies that benefit the greatest public good.”
Through papers, presentations, and panel discussions, the center last year also contributed ethical content to debates over legalizing assisted suicide in the United States and the United Kingdom, the use of psychedelic medicine, interstate and federalism conflicts in abortion law following the U.S. Supreme Court’s elimination of a national right to an abortion, overconsumption of acute care resource at end of life, and how to support medical researchers and patients who fled Ukraine while conducting or participating in drug trials. And the center’s Community Bioethics Forum continued to lead in the creation of innovative methods to amplify the voices and values of communities within health policy, influencing law and policy in Connecticut and nationwide.
“As science addresses the challenges ahead, the center will continue to advance its vital work across all Yale departments and professional schools,” Latham said. “As well as political, economic, and religious institutions. Our goal is to generate improved understanding, develop an informed citizenry, and enable thoughtful public and private debate and action.”